Multidisciplinary PWS care often follows GH-treated children into adulthood
These children were also less likely to develop obesity-related complications later
Written by |
Adults with Prader-Willi syndrome (PWS) who were given growth hormone (GH) therapy in childhood are more likely to continue to be monitored by a multidisciplinary care team, according to results from a survey conducted in Japan.
“These results emphasize the importance of the seamless provision of the multidisciplinary team approach, which is of clinical importance for establishing an optimal transitional care program for PWS,” researchers wrote.
Receiving growth hormone therapy during childhood is also associated with fewer obesity-related complications, such as type 2 diabetes and high blood pressure, later in life.
The study, “A questionnaire-based survey of medical conditions in adults with Prader-Willi syndrome in Japan: implications for transitional care,” was published in the Endocrine Journal.
Obesity associated with host of health problems
PWS is a rare genetic disease whose symptoms commonly include an excessive appetite, leading to obesity and obesity-related conditions, developmental delays and behavioral abnormalities, as well as shorter stature.
Because obesity and its effects are associated with a host of health problems, management for PWS is mostly focused on approaches that help change body composition. These include nutritional interventions and GH therapy — which promotes growth, increases muscle mass and tone, and lowers body fat.
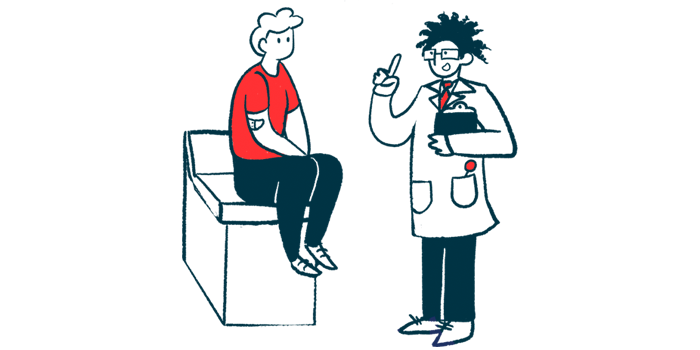
Managing obesity-related complications in children diagnosed with PWS has been deemed more effective when patients are followed by a multidisciplinary team that includes pediatric endocrinologists, dietitians, nurse practitioners, geneticists, and psychologists.
However, this approach is more challenging to implement during adulthood, due to the lack of transitional programs transferring care from pediatric to adult services. The fact that PWS affects multiple systems, requiring management from several specialists, is one of the main roadblocks in this transition, according to the researchers.
GH therapy during childhood was associated with a lower frequency of obesity-related complications during adulthood.
Study included 425 adults, 73% of whom were treated with GH during childhood
To determine how to provide better transitional care to people with PWS entering adulthood, a team of researchers in Japan conducted a questionnaire-based survey to understand the disease in adults and how that transition happened for them.
The survey included 425 patients who were registered in the country’s PWS association. Their median age was 14 years, and 162 were adults. The majority (93.4%) were diagnosed based on genetic testing, which was mostly conducted early after birth or during infancy.
A total of 308 patients (72.8%) were treated with growth hormone during childhood, and two patients also received GH therapy during adulthood.
About 17% of patients had type 2 diabetes, 7.7% had high blood pressure, and 15.6% had sleep apnea, in which breathing repeatedly stops during sleep. Scoliosis, an abnormal curvature of the spine, was reported in 31.7% of patients.
Adult patients were more likely to develop diabetes (40.4%) and high blood pressure (19.4%), which were particularly more common in those who were obese — with a body mass index above 25.
Fewer people who received GH therapy during childhood developed these complications, the team noted, with 30.4% developing diabetes and 8.9% developing high blood pressure, compared with 55.2% and 33.3% for those who were not given GH when they were children.
Multidisciplinary approach commonly used with GH therapy
Information on healthcare providers was available for 160 adult patients. The majority (157 patients) were regularly followed by physicians — 54.4% by pediatricians, 43.8% by internists, and 11.3% by both pediatricians and internists. Among internists, the most commonly seen were endocrinologists and diabetologists (diabetes specialists).
Other specialties included psychiatrists or psychotherapists (38.1%), orthopedists (28.8%), and dermatologists (27.5%).
More GH-treated patients (63%) were seen by pediatricians in adulthood compared with those who were not treated with GH as children (45%).
Overall, these findings suggest that a multidisciplinary approach that is commonly used with GH therapy is available to PWS patients in adulthood, according to the researchers.
“GH therapy during childhood was associated with a lower frequency of obesity-related complications during adulthood,” they added.
“Although the underlying mechanisms remain unclear, we assume that the multidisciplinary team approach, which is generally applied to patients treated with GH, is continuously provided to these patients even after they enter adulthood,” the team concluded.